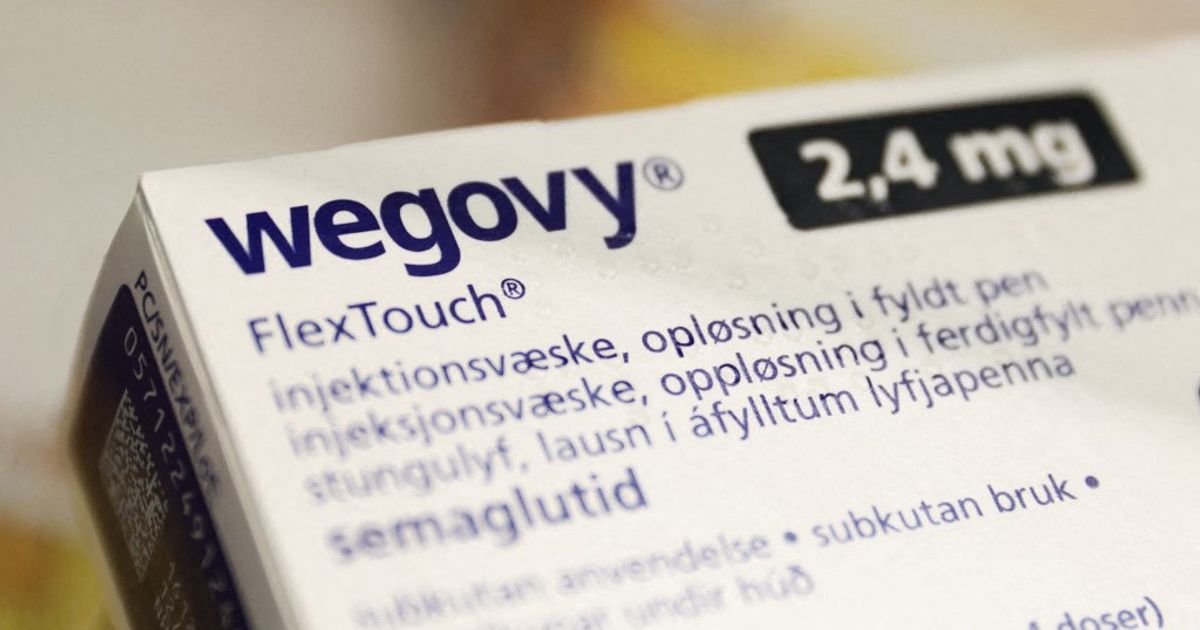
Weight loss medications, particularly injectable peptides like semaglutide (Wegovy, Ozempic), liraglutide (Saxenda), and tirzepatide (Mounjaro), have shown remarkable success in helping individuals reduce body weight. These drugs, known as GLP-1 receptor agonists, work by regulating blood sugar and suppressing appetite, often prescribed for those with a BMI over 30, or between 27 and 29 with additional health risks like pre-diabetes, hypertension, or cardiovascular disease. However, maintaining weight loss achieved through these therapies can be a significant challenge, often requiring long-term, even lifelong, treatment, which can be costly.
Clinical research indicates that discontinuing GLP-1 agonist therapy frequently leads to a rapid return of lost weight. While some individuals maintain their results through sustained lifestyle changes, the long-term effects after cessation, including impacts on cardiovascular health and metabolism, remain under investigation. It's also unclear which strategies best prevent weight regain, the optimal duration of therapy, or the criteria for determining when to continue or discontinue treatment for sustained success.
Internal medicine and endocrinology specialist Davorka Herman Mahečić emphasizes the "yo-yo" effect often observed after stopping these medications, explaining that the brain resists weight loss, and hunger returns when the appetite-regulating effects of the drugs are gone. Obesity, according to the World Health Organization, is a chronic disease that requires ongoing management. Some patients may require lifelong medication, a strategy that aims to gradually reduce therapy under medical supervision while monitoring symptoms, particularly hunger.
She recommends focusing on dietary habits and physical activity, recommending nutritional counseling to prioritize protein intake and encourage regular exercise. She also cautions that Ozempic is primarily intended for treating type 2 diabetes and should not be promoted solely as a weight loss drug.